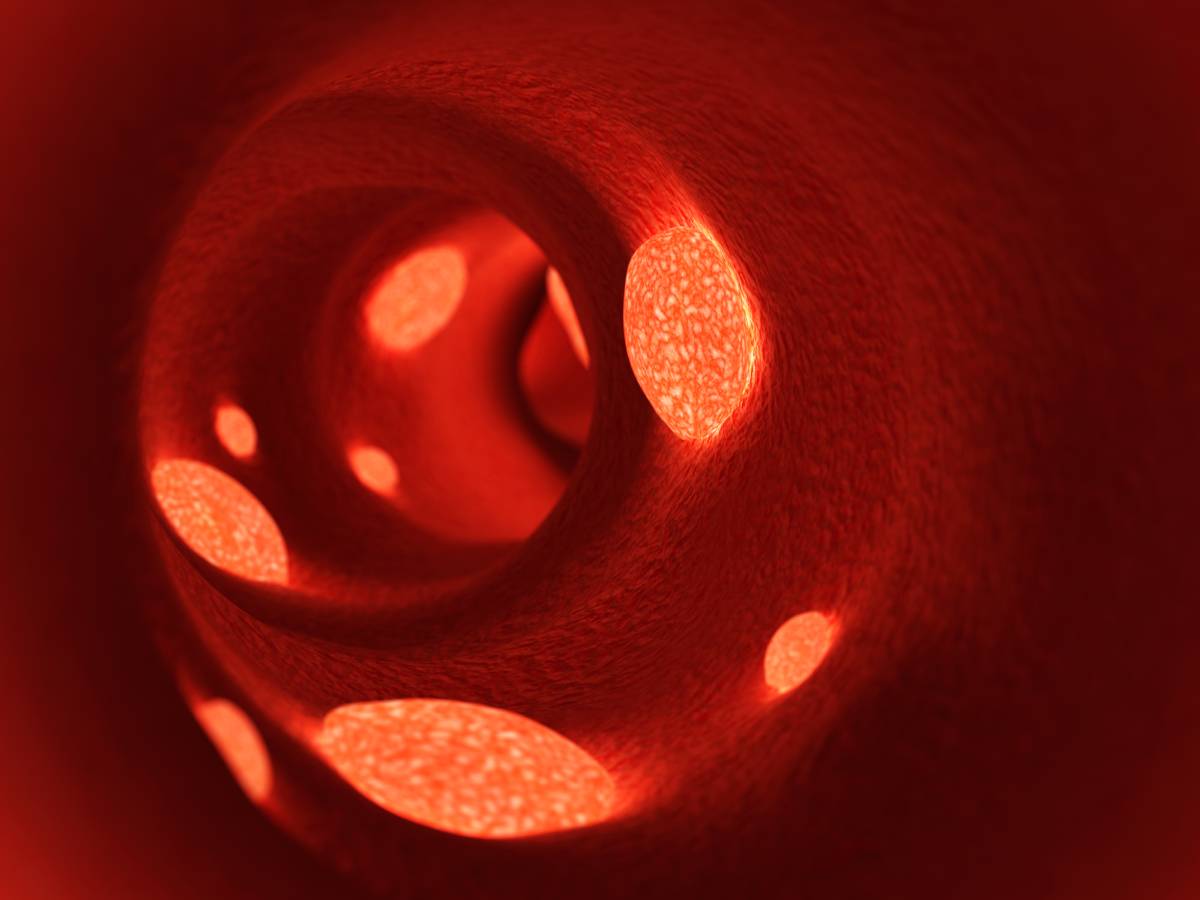
Disseminated intravascular coagulation (DIC) is a serious condition characterized by the occurrence of diffuse microthrombi in small blood vessels [1]. DIC happens in the presence of underlying disease and is also associated with fibrin deposition that increases the risk of multiple organ injury [1]. Progressive DIC may result in exhaustion of coagulation proteases and platelets, leading to an increased chance of hemorrhagic complications [2]. Therefore, DIC often presents as a simultaneous thrombotic and bleeding issue [3].
DIC is not considered a distinct disease diagnosis, but instead a sign of underlying illness [3]. The most common clinical conditions linked to DIC are sepsis, acute leukemia, and solid cancers [1]. However, there are a variety of other conditions that have been associated with DIC, such as severe infections, trauma, burns, heat stroke, surgery, abdominal aortic aneurysm, connective tissue disease, acute pancreatitis, shock, and giant hemangioma [1,3].
A diagnosis of DIC should only be made in the presence of an underlying clinical condition supported by relevant laboratory findings [3]. The pathogenesis (especially relating to the degree of fibrinolytic activation) of DIC differs considerably depending on the underlying condition [1]. DIC is classified as (1) DIC with suppressed fibrinolysis, (2) DIC with enhanced fibrinolysis, or (3) DIC with balanced fibrinolysis [1]. Marked activation of coagulation is a key pathogenic factor in DIC and is common to all DIC types [1].
DIC with suppressed fibrinolysis is characterized by severe coagulation activation and mild fibrinolytic activation [1]. It is typically seen in cases of sepsis [1]. Laboratory findings include significant elevation in coagulation activation markers but only mild elevation in fibrinolysis activation markers [1]. In contrast, DIC with enhanced fibrinolysis is associated with marked coagulation and fibrinolysis activation [1]. It is typically seen in abdominal aortic aneurysm and prostate cancer [1]. Laboratory findings reveal an elevation in coagulation and fibrinolysis activation markers, as well as D-dimer levels [1]. DIC with balanced fibrinolysis manifests as an intermediate pathogenesis [1]. It is common in solid cancers and may progress to DIC with enhanced fibrinolysis in some cases [1].
Proper DIC management involves treatment of the underlying clinical condition, such as administration of antibiotics in patients with infections or anticancer therapies in patients with cancer [4]. DIC has been shown to spontaneously resolve in cases where the underlying condition was effectively treated [4]. Patients with DIC may require blood transfusions due to dangerously low levels of platelets and coagulation factors that increase the risk of bleeding [4]. Administration of platelet concentrate and fresh frozen plasma in DIC patients has been associated with positive outcomes [4]. Anticoagulant treatment is also considered in cases of DIC in which thrombosis predominates [4]. Therapeutic doses of low molecular weight heparin have been administered to DIC patients at risk for venous thrombotic events [4].
Although current therapeutic interventions for disseminated intravascular coagulation can lead to improvement in coagulopathy and rapid resolution of DIC, they have not been shown to affect clinically relevant outcomes like organ dysfunction or mortality [5]. Management of DIC may benefit from refined treatment approaches that target organ systems that are most affected [5]. Moreover, efforts toward early patient identification and risk stratification would allow for earlier intervention and prevent development of uncontrolled disseminated intravascular coagulation [5].
References
- Asakura, H. (2014). Classifying types of disseminated intravascular coagulation: clinical and animal models. Journal of Intensive Care, 2(1), 1-7. doi:10.1186/2052-0492-2-20
- Levi, M. (2014). Diagnosis and treatment of disseminated intravascular coagulation. International Journal of Laboratory Hematology, 36(3), 228-236. doi:10.1111/ijlh.12221
- Venugopal, A. (2014). Disseminated intravascular coagulation. Indian Journal of Anaesthesia, 58(5), 603. doi:10.4103/0019-5049.144666
- Wada, H., Matsumoto, T., & Yamashita, Y. (2014). Diagnosis and treatment of disseminated intravascular coagulation (DIC) according to four DIC guidelines. Journal of Intensive Care, 2(1), 1-8. doi:10.1186/2052-0492-2-15
- Gando, S., Levi, M., & Toh, C. (2016). Disseminated Intravascular Coagulation. Nature Reviews Disease Primers, 2(1). doi:10.1038/nrdp.2016.37